Minimally Invasive Surgery for Joint Preservation
Hip Arthroscopy
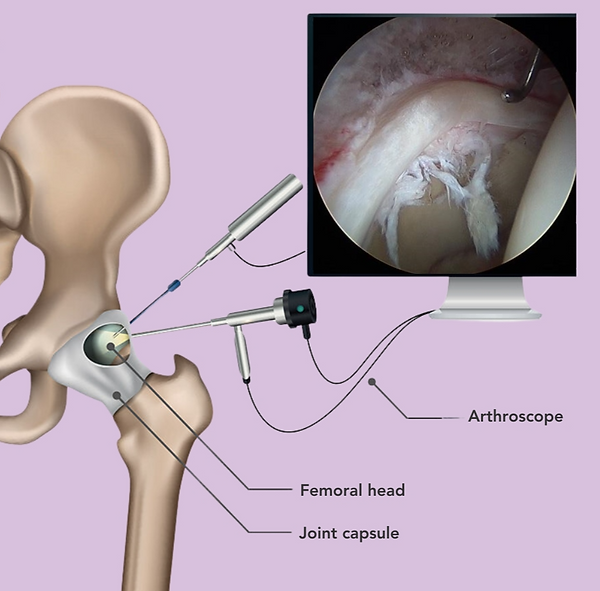
Hip arthroscopy is a modern, minimally invasive procedure used to diagnose and treat a variety of hip conditions—without the need for joint replacement. Through small incisions and fiber-optic tools, surgeons can repair damaged cartilage, reshape bone, and relieve painful impingement.
The goal? To restore mobility, reduce pain, and preserve your natural joint for as long as possible. Whether you’re an athlete with a labral tear or someone struggling with persistent hip pain, hip arthroscopy may be a game-changing step toward long-term relief.
What Is Hip Arthroscopy?
Hip arthroscopy is a minimally invasive surgical procedure that allows your surgeon to access and treat the inside of the hip joint using small incisions and a fiber-optic camera. Unlike open surgery or joint replacement, arthroscopy is focused on preserving your natural hip—not replacing it.
During the procedure, your surgeon uses a small scope and specialized instruments to:
-
Visualize the joint in real time
-
Remove or repair damaged tissue
-
Reshape areas of bone that are causing impingement
-
Restore function while minimizing trauma to surrounding structures
Why It's Different From Traditional Hip Surgery
Traditional hip surgeries often involve large incisions, longer recovery times, and greater disruption of healthy tissue. In contrast, hip arthroscopy typically uses two to three incisions, each less than 1 inch long, and is performed on an outpatient basis.
Patients can usually:
-
Go home the same day
-
Begin physical therapy within a week
-
Return to full activity in 3–4 months depending on the case
Think of hip arthroscopy as a precision tool—not a full replacement. It’s about fixing the issue while keeping the joint you were born with.
Conditions Treated with Hip Arthroscopy
Hip arthroscopy is often recommended when conservative treatments like physical therapy, injections, or rest haven’t resolved symptoms—and imaging shows that a structural problem inside the joint needs to be addressed.
This procedure is highly effective for treating labral injuries and correcting mechanical issues that cause pain, instability, or early joint damage.
Common Conditions Treated with Hip Arthroscopy:
-
Labral tears
Arthroscopy allows your surgeon to repair or reconstruct the labrum—a ring of cartilage that stabilizes the hip socket. -
Femoroacetabular impingement (FAI)
Cam or pincer lesions (bone overgrowths) are shaved down to prevent future damage and relieve joint stress. -
Cartilage damage or delamination
Damaged cartilage can be smoothed, repaired, or stimulated to heal using techniques like microfracture. -
Loose bodies
Arthroscopy can remove bone or cartilage fragments floating in the joint that cause locking or catching. -
Ligamentum teres injuries
Partial or complete tears of this internal hip ligament can be debrided or treated to reduce instability. -
Early synovitis or inflammation
Inflamed joint lining tissue can be cleaned out to improve pain and joint motion.
In some cases, especially in younger patients with hip dysplasia, hip arthroscopy may be combined with procedures like periacetabular osteotomy (PAO) to correct socket alignment while addressing intra-articular damage. This combined approach helps preserve the joint more effectively in the long term.
Hip arthroscopy is not just for elite athletes—it’s for anyone whose joint mechanics or cartilage health need expert attention without the invasiveness of open surgery.
The Procedure – Step by Step
Hip arthroscopy is typically performed under general anesthesia and takes between 60 and 120 minutes, depending on your specific condition and what needs to be addressed inside the joint.
Unlike traditional open surgery, this minimally invasive technique allows your surgeon to access the joint through two to three tiny incisions, using a fiber-optic camera and specialized instruments. The goal is to identify and treat the root cause of your hip pain while minimizing disruption to the surrounding tissues.
Review our step-by-step preparation guide to know what to expect before surgery
What Happens During Hip Arthroscopy:
1. Positioning & Joint Access
You’ll be positioned on a specialized traction table to gently separate the femoral head from the socket, creating enough space to safely insert instruments into the joint. Depending on your surgeon’s technique, this may be done using a traditional perineal post or a newer post-free method (more on this in the next section).
Careful positioning is critical to protect surrounding nerves and ensure a safe, effective procedure.
2. Portal Placement
The surgeon makes two or three small incisions—usually less than 1 inch long—on the outer side of the hip. These are called arthroscopic portals and allow access to the joint without cutting through major muscles or tendons.
One portal is used to insert a small camera (arthroscope), while the others allow surgical instruments to treat the damage inside the joint.
3. Diagnostic Assessment
Once the camera is inside, the surgeon inspects the entire hip joint to identify:
-
Bone spurs (cam or pincer lesions)
-
Cartilage damage
-
Ligament injuries or inflammation
-
Loose bodies or synovitis
Often, imaging like MRI provides a preliminary diagnosis, but arthroscopy allows real-time, detailed visualization to confirm what needs to be addressed.
4. Treatment & Repair
Based on what’s found, your surgeon will:
-
Repair or reconstruct the labrum to restore the suction seal of the hip
-
Reshape bone to correct femoroacetabular impingement (FAI)
-
Treat cartilage damage using techniques like debridement or microfracture
-
Remove loose fragments or inflamed tissue (synovectomy)
-
Address instability from ligamentum teres tears or capsular laxity
5. Closing & Recovery
Once the procedure is complete, the instruments are removed, and the portals are closed with small sutures or adhesive strips. You’ll then be moved to recovery and typically discharged within a few hours.
Most patients return home the same day with crutches, a structured rehab plan, and post-op instructions for pain management and mobility.
Hip arthroscopy is both a diagnostic and therapeutic tool—designed to treat the source of your pain while preserving the natural structure of your hip.

Modern Techniques – Post-Free Arthroscopy
Traditional hip arthroscopy has historically required the use of a perineal post—a padded support placed between the patient’s legs—to create traction and open space in the hip joint. While effective, this technique has been associated with a small but real risk of complications, including:
-
Genital numbness
-
Soft tissue compression
-
Nerve irritation
-
Perineal discomfort after surgery
To minimize these risks, many modern hip surgeons now perform post-free hip arthroscopy—an advanced technique that eliminates the need for a perineal post altogether.
🚫 What Is Post-Free Arthroscopy?
Instead of relying on a central post, this technique uses a specialized table and body positioning to apply traction more safely and evenly across the patient’s body. This approach:
-
Reduces pressure on sensitive nerves and soft tissue
-
Lowers the risk of traction-related complications
-
Improves overall comfort and safety during surgery
Post-free arthroscopy represents a major advancement in patient-centered surgical care, especially for younger, athletic patients who prioritize both performance and safety.
✅ Benefits of the Post-Free Technique:
-
Minimizes risk of perineal nerve injury
-
Avoids genital discomfort or bruising
-
Allows for more natural hip positioning
-
Enhances patient confidence in the surgical experience
Recovery Timeline After Hip Arthroscopy
Recovery after hip arthroscopy is a gradual, phased process that depends on the specific procedure performed, your overall health, and your goals. Most patients begin walking with assistance within a few days and progress to light activity within several weeks.
Here’s what a typical recovery timeline looks like:

Key Reminders:
-
Progress is gradual—rushing the process increases the risk of reinjury
-
Your recovery plan will be customized based on your procedure (e.g., labral repair vs. bone reshaping)
-
Working with a hip-specific physical therapist is essential for long-term results
Most patients are walking unassisted by 4–6 weeks and back to full activity within 3–4 months.
_edited.jpg)
Rehabilitation & Physical Therapy
Physical therapy is a critical part of the recovery process after hip arthroscopy. While surgery addresses the structural problem inside the joint, rehabilitation restores mobility, strength, and stability—helping you return to your lifestyle safely and confidently.
What Makes Hip Rehab Different?
The hip is a deep, complex joint surrounded by powerful muscles. Recovering from arthroscopy requires a structured, phase-based rehab plan that addresses both movement and muscle balance.
Your physical therapist will guide you through each phase:
Typical Phases of Post-Arthroscopy Rehab
-
Protection Phase (Weeks 1–2)
-
Focus: Reducing pain and inflammation
-
Gentle mobility exercises, limited weight-bearing, and icing protocols
-
-
Mobility + Activation (Weeks 3–6)
-
Begin range-of-motion training and light muscle activation
-
Focus on glutes, core, and deep stabilizers
-
-
Strength + Control (Weeks 6–10)
-
Progressive loading of the hip joint with resistance training
-
Balance and gait retraining
-
-
Return to Sport/Activity (Weeks 10–16+)
-
Sport-specific drills, agility, impact control
-
Ongoing flexibility, posture, and movement optimization
-
Our rehab tips blog covers strategies that help patients return to sports sooner.
Is a Brace Required After Hip Arthroscopy?
In most cases, no brace is required after hip arthroscopy. While some surgeons may recommend a post-operative hip brace to limit movement or support healing, research has shown that routine bracing provides minimal added benefit for most patients.
❌ Why We Typically Avoid Bracing:
-
Braces can be bulky, uncomfortable, and expensive
-
They may restrict mobility unnecessarily and delay progress
-
There’s limited evidence that braces improve surgical outcomes after arthroscopy
Instead, we focus on:
-
Controlled weight-bearing using crutches in the early phase
-
Personalized physical therapy to restore safe movement patterns
-
Clear movement guidelines provided by your care team
In the vast majority of cases, active rehabilitation is more effective than external bracing.
When a Brace Might Be Considered:
-
If the patient has significant joint instability
-
In rare cases of concurrent procedures (e.g., capsular reconstruction or instability surgery)
-
Based on surgeon preference or patient-specific factors
✅ What You’ll Need After Hip Arthroscopy
-
☐ Crutches (for 1–2 weeks depending on weight-bearing instructions)
-
☐ Ice packs or cold therapy unit for swelling and pain control
-
☐ Loose, comfortable clothing that’s easy to put on post-surgery
-
☐ Pre-arranged transportation for your surgery day and first follow-ups
-
☐ Physical therapy appointments scheduled in advance
-
☐ Elevated seating or shower bench (optional for added comfort)
-
☐ Prescribed medications for pain and inflammation
-
☐ A recovery timeline—so you know what progress looks like week to week
-
☐ A positive mindset and a dedicated support system
Most importantly, you’ll need a structured plan and a care team that specializes in hip preservation and recovery.
Success Rates & Long-Term Outcomes
Hip arthroscopy has an excellent track record when performed on the right patient, for the right condition, with a personalized rehab plan. In fact, research shows that 80–95% of patients experience significant pain relief, improved function, and return to activity following surgery.
What Influences Success?
Several factors impact the long-term results of hip arthroscopy, including:
-
Age – Patients under 40 tend to have better outcomes due to healthier cartilage and faster healing
-
Extent of joint damage – Labral tears or mild FAI respond better than advanced arthritis
-
Timing of surgery – Addressing issues early helps prevent irreversible joint damage
-
Rehab participation – Following the post-op rehab plan is crucial for sustained improvement
-
Presence of arthritis – Outcomes are more limited if moderate to severe arthritis is already present
When structural problems like FAI or labral tears are treated before permanent joint damage sets in, hip arthroscopy can delay or even prevent the need for hip replacement surgery.
🏋️ Get Strong Before Surgery
Prehab matters. Building strength and mobility before hip surgery can improve your outcome and speed up recovery.
Explore our blog: Top Exercises to Prepare for Hip Surgery ›
How Long Do Results Last?
-
Most patients report benefits lasting 7–10 years, or longer
-
Some may eventually need a follow-up procedure or joint replacement if arthritis progresses
-
For active patients, arthroscopy often restores confidence and performance levels that were lost to chronic pain

Who Is a Candidate for Hip Arthroscopy?
Hip arthroscopy is a highly effective procedure—but it’s not for everyone. The best candidates are typically younger, active individuals with specific structural problems that haven’t responded to conservative treatment.
This minimally invasive surgery is intended to preserve the natural joint and should ideally be done before significant arthritis sets in.
You May Be a Good Candidate If You:
-
Are under 40 (though select patients in their 40s–50s may still benefit)
-
Have persistent groin or outer hip pain
-
Have a confirmed diagnosis of a labral tear, FAI, or related intra-articular condition
-
Have minimal to no arthritis on imaging
-
Have tried conservative treatments (PT, injections) without relief
-
Are motivated to follow a structured rehab program
Adolescents and young athletes with hip impingement often start with subtle signs. See our parent’s guide here.
You May Not Be a Candidate If You:
-
Have moderate to severe hip arthritis
-
Have diffuse, non-specific hip pain without clear imaging findings
-
Are unable to participate in post-op rehab due to other health factors
-
Are primarily seeking pain relief from arthritis rather than mechanical correction
For certain hip conditions, PAO may be a better fit. Here’s how PAO compares to hip arthroscopy.
🤔 Still Unsure About Hip Arthroscopy?
Before committing to surgery, it’s smart to get all the facts.
We offer second opinions to help patients confirm their diagnosis, evaluate non-surgical options, or explore the timing of arthroscopy.
A fresh perspective could give you the confidence to move forward—or wait.
Are You a Good Candidate for Hip Arthroscopy?
Determining if hip arthroscopy is right for you depends on several factors, including your age, diagnosis, the extent of structural damage, and the presence of arthritis. The procedure tends to have the best outcomes in individuals under 40 years old with minimal arthritis and specific structural issues. A comprehensive evaluation is necessary to assess your unique condition and determine whether hip arthroscopy is the best treatment option for your goals and lifestyle.
To help you get started, take the "Are You a Surgical Candidate?" quiz on our webpage. This tool can provide preliminary insights into whether hip arthroscopy might be suitable for your condition and guide the next steps in your journey to hip health.
Take the Next Step Toward Hip Relief
Hip arthroscopy offers a modern, minimally invasive solution for active individuals dealing with labral tears, impingement, or persistent hip pain. If conservative treatments haven’t worked—and you want to preserve your natural joint while getting back to the activities you love—this procedure could be the right fit.
At HipPreservation.org, our team is here to guide you every step of the way.
Ready to Start?
Get the answers, treatment, and expert guidance you deserve. Your hip health starts here.

.png)
